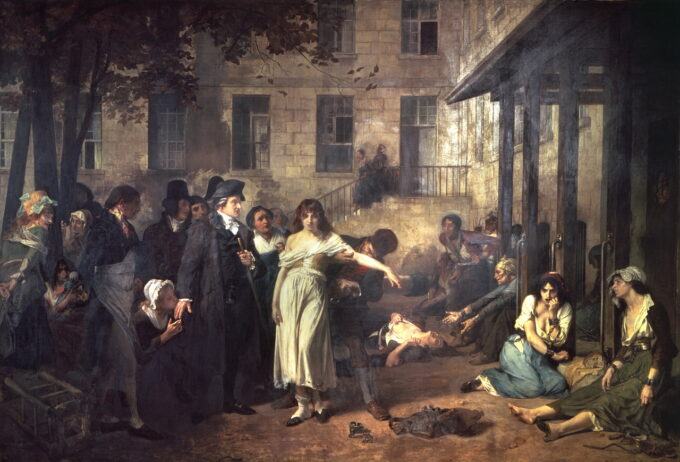
French psychiatrist Philippe Pinel (1745-1826) releasing lunatics from their chains at the Salpêtrière asylum in Paris in 1795 – Public Domain
One need not be a Marxist to acknowledge the logic behind Karl Marx’s observation: “The ideas of the ruling class are in every epoch the ruling ideas.” It is especially important for the ruling class that the general public’s ideas about our emotional suffering and behavioral disturbances be the ideas of the ruling class.
Twenty years ago, one would have been labeled as “anti-psychiatry” for acknowledging that: (1) psychiatry’s treatment outcomes are “abysmal” and “not getting any better”; (2) the serotonin imbalance theory of depression is untrue; and (3) psychiatry’s diagnostic manual, the DSM, is scientifically invalid. Yet today, these acknowledgements—which don’t threaten the ruling class—are stated by the psychiatry establishment and reported by the mainstream media.
There are, however, critiques that continue to be too taboo for the mainstream media to report. Such critiques are existential threats to establishment psychiatry, and these critiques are financial threats to both Big Pharma and a mainstream media dependent on Big Pharma advertising dollars. Even more importantly, these critiques are political threats to the ruling class which prefers medical “individual defect” explanations for emotional suffering and behavioral disturbances rather than explanations that challenge the societal status quo.
Once Radical Critiques That Are Now Mainstream
Treatment Outcome Failure: In 2011, Thomas Insel, director of the National Institute of Mental Health (NIMH) from 2002-2015, acknowledged: “Whatever we’ve been doing for five decades, it ain’t working. When I look at the numbers—the number of suicides, the number of disabilities, the mortality data—it’s abysmal, and it’s not getting any better.” In 2017, Insel told Wired: “I spent 13 years at NIMH really pushing on the neuroscience and genetics of mental disorders, and when I look back on that I realize that while I think I succeeded at getting lots of really cool papers published by cool scientists at fairly large costs—I think $20 billion—I don’t think we moved the needle in reducing suicide, reducing hospitalizations, improving recovery for the tens of millions of people who have mental illness.” In 2021, New York Times reporter Benedict Carey, after covering psychiatry for twenty years, concluded that psychiatry had done “little to improve the lives of the millions of people living with persistent mental distress. Almost every measure of our collective mental health—rates of suicide, anxiety, depression, addiction deaths, psychiatric prescription use—went the wrong direction, even as access to services expanded greatly.” While twenty years ago, it would have been radical to state that psychiatry is making no progress, today it is not taboo to report that our collective mental health has gone in “the wrong direction” despite increased treatment.
No Scientific Basis for the Serotonin Imbalance Theory of Depression. In 2022, CBS reported: “Depression is Not Caused by Low Levels of Serotonin, New Study Suggests.” Receiving widespread attention in the mainstream media was the July 2022 research review article “The Serotonin Theory of Depression: A Systematic Umbrella Review of the Evidence,” published in the journal Molecular Psychiatry. In it, Joanna Moncrieff, co-chairperson of the Critical Psychiatry Network, and her co-researchers examined hundreds of different types of studies that attempted to detect a relationship between depression and serotonin, and concluded that there is no evidence of a link between low levels of serotonin and depression, stating: “We suggest it is time to acknowledge that the serotonin theory of depression is not empirically substantiated.” Leading establishment psychiatrists, rather than disputing these finding, tried to convince the general public that Moncrieff’s findings were not newsworthy.
Invalidity of Psychiatry’s Diagnostic Manual. Key members of establishment psychiatry now acknowledge that the DSM, psychiatry’s diagnostic manual, is invalid. Thomas Insel, when NIMH director in 2013, stated that the DSM’s diagnostic categories lack validity, and he announced that “NIMH will be re-orienting its research away from DSM categories.” Then, in his 2022 book Healing, Insel stated: “The DSM had created a common language, but much of that language had not been validated by science.” The chair of the 1994 DSM-IV task force, Allen Frances, acknowledged in 2010 that “there is no definition of a mental disorder. It’s bullshit. I mean, you just can’t define it.” Not only does the DSM lack validity, in 2012, Frances detailed how DSM diagnoses lack reliability, as different clinicians rating the same patient routinely disagree on a diagnosis.
What Remains Taboo Criticism of Psychiatry?
What remains taboo is criticism of psychiatry that calls into question its fundamental paradigm of care. Specifically, this means it is taboo to ask this question: Has viewing our emotional suffering and behavioral disturbances as medical disorders and illnesses been helpful or harmful? Thus, the mainstream media rarely reports the empirical research that challenges psychiatry’s essential paradigm—its so-called “medical model.”
In psychiatry’s medical model, mental illnesses and their symptoms are voted in by the American Psychiatric Association (APA), and then listed in the DSM, published by the APA. DSM mental illnesses such as attention deficit hyperactivity disorder (AHDH) and schizophrenia are—like gonorrhea and cancer—seen as pathological conditions. While psychiatry generally views mental illnesses as biological in nature—be it chemical imbalances (now a discarded theory) or other theories involving brain and genetic defects—its medical model, as in much of the rest of medicine, does not preclude the effect of psychological and social factors on biological functioning. (Just as oncologists embrace the idea that genetics predisposes a person to cancer but recognize that psychological and social variables can trigger it, so too does psychiatry’s medical model recognize that psychosocial variables can trigger DSM mental illnesses.)
In contrast to psychiatry’s medical model, other models of emotional suffering and behavioral disturbances don’t assume that a medical illness is causing emotional suffering or disturbing behaviors. Non-medical models conclude that there are many reasons that have nothing to do with medical illness as to why, for example, a child does not pay attention and is disruptive; and such non-medical models conclude there are many reasons that have nothing to do with brain defects as to why an individual may be hearing voices and having bizarre beliefs.
Before examining the research that casts doubt on the neurobiological validity of psychiatry’s medical model, first the empirical research that examines whether or not the medical model creates more or less stigma.
Has Psychiatry’s Medical Model Created More or Less Stigma? In 2006, Acta Psychiatrica Scandinavica published “Prejudice and Schizophrenia: A Review of the ‘Mental Illness is an Illness Like Any Other’ Approach,” lead authored by psychologist John Read. The review examined several studies that looked at whether labeling someone with a medical illness such as “schizophrenia,” rather than describing them non-medically as “in crisis,” was associated with more or less negative attitudes. These studies conclude that labeling behaviors as “schizophrenia” increases the belief in biological causality and increases the perceived seriousness of the person’s difficulties, which produces a more pessimistic view about recovery. Moreover, if a person is seen as having the serious mental illness of schizophrenia, the public more desires to keep their distance from them rather than if the person is seen as “in crisis”; in other words, medicalization creates more stigma.
Examining twenty-one studies, Read found that biological-genetic causal beliefs are clearly associated with more negative attitudes: “From 1970, studies in several industrialized countries have found that biogenetic causal beliefs are related to negative attitudes. This has been demonstrated among patients and professionals as well as general populations. Biogenetic beliefs are related to perceptions of dangerousness and unpredictability, to fear, and to desire for social distance.” The research clearly shows that the brain disease conceptualization and the “an illness like any other” anti-stigma campaign have resulted in greater stigmatization.
Similarly, in “Myth: Reframing Mental Illness as a ‘Brain Disease’ Reduces Stigma,” the Canadian Health Services Research Foundation (CHSRF) reported in 2012: “Despite good intentions, evidence actually shows that anti-stigma campaigns emphasizing the biological nature of mental illness have not been effective, and have often made the problem worse.” The CHSRF concludes, “Biological explanations can also instill an ‘us vs. them’ attitude, defining individuals with mental illness as fundamentally different.”
But Haven’t Brain Scans and Genetic Research Proven Brain Disease? Published in the journal Neuron in 2022, Raymond Dolan—considered one of the most influential neuroscientists in the world—co-authored “Functional Neuroimaging in Psychiatry and the Case for Failing Better,” concluding, “Despite three decades of intense neuroimaging research, we still lack a neurobiological account for any psychiatric condition.” Reflecting on the more than 16,000 neuroimaging articles published during the last 30 years, Dolan and his co-authors concluded: “It remains difficult to refute a critique that psychiatry’s most fundamental characteristic is its ignorance. . . . Casting a cold eye on the psychiatric neuroimaging literature invites a conclusion that despite 30 years of intense research and considerable technological advances, this enterprise has not delivered a neurobiological account (i.e., a mechanistic explanation) for any psychiatric disorder, nor has it provided a credible imaging-based biomarker of clinical utility.”
What about genetic correlates to “serious mental illnesses”? A 2020 study in Schizophrenia Bulletin reported that no genetic variants have been found to predict schizophrenia; as no significant difference was found in the genetic variance of people with a diagnosis of schizophrenia and people without such a diagnosis. Similarly, examining mood disorders, a 2021 investigation published in the Journal of Affective Disorders (that included 5,872 cases and 43,862 controls, and examined 22,028 genes), reported that the study “fails to identify genes influencing the probability of developing a mood disorder” and “no gene or gene set produced a statistically significant result.”
Thus, despite the fact that researchers have not found any neuro-chemical-biological-genetic evidence for any psychiatric condition, it remains taboo to challenge psychiatry’s medical model and brain disease ideas about emotional suffering and behavioral disturbances.
But Haven’t Psychiatric Treatments Been Helpful for Millions of People? For nearly three thousand years, individuals diagnosed as mad or insane were given the treatment of bloodletting, and many of these individuals and their physicians reported improvement. In the modern scientific era, it is recognized that improvements may follow after any treatment, and so researchers attempt to tease out whether those improvements are the result of mere expectations (the placebo effect) and the passage of time, or whether the specific treatment actually had a significant effect.
In April 2002, the Journal of the American Medical Association (JAMA) published a study that investigated whether the herb St. John’s wort, purported to be an antidepressant, was more effective than a placebo. In this randomized controlled trial (RCT), in addition to one group given St. John’s wort and a second group given a placebo, there was a third group that received the standard dose of the SSRI Zoloft. The results? The placebo worked better than both St. John’s wort and Zoloft. Specifically, a positive “full response” occurred in 32 percent of the placebo-treated patients, 25 percent of the Zoloft-treated patients, and 24 percent of the St. John’s wort-treated patients.
This study—showing that a placebo was more effective than both St. John’s wort and Zoloft—was published with the tile, “Effect of Hypericum perforatum (St John’s wort) in Major Depressive Disorder: A Randomized Controlled Trial,” begging the question as to why there was no mention of Zoloft in the study title. Zoloft is manufactured by Pfizer, and the financial disclosure of the above study’s lead author, psychiatrist Jonathan R. T. Davidson, states: “Dr. Davidson holds stock in Pfizer [manufacturer of Zoloft] . . . and has received speaker fees from Pfizer.”
But aren’t there other RCT studies that show that Zoloft and other antidepressants to be more effective than a placebo? A leading researcher of the placebo effect is psychologist Irving Kirsch, and in 2002, Kirsch examined forty-seven drug company studies on various and other antidepressants. These studies included published and unpublished trials, but all had been submitted to the Food and Drug Administration (FDA), so Kirsch used the Freedom of Information Act to gain access to all data. He discovered that in the majority of the trials, antidepressants failed to outperform placebos, and he reported that “all antidepressants, including the well-known SSRIs . . . had no clinically significant benefit over a placebo.” While in aggregate, antidepressants slightly edged out placebos, the difference is so unremarkable that Kirsch and others describe it as “clinically negligible.”
Long-term antidepressant outcomes are even worse. Drug companies are not required to do long-term outcome studies to acquire FDA approval; as the FDA’s “Major Depressive Disorder: Developing Drugs for Treatment Guidance for Industry” states the following: “Antidepressants in established classes (e.g., SSRIs, SNRIs) typically need studies of 6 to 8 weeks duration to demonstrate efficacy.” Thus, the general public is unaware of studies that show antidepressants, over the long term, may result in more, not less, depression. In 2017, “Poorer Long-Term Outcomes among Persons with Major Depressive Disorder Treated with Medication,” published in Psychotherapy and Somatics, reported that controlling for depression severity, the outcomes of 3,294 subjects over a nine-year period showed that antidepressants may have had an immediate, short-term benefit for some people, but at the nine-year follow-up, antidepressant users had significantly more severe symptoms than those individuals not using antidepressants.
How effective are antipsychotic drugs used on individuals diagnosed with schizophrenia? In an NIMH-funded study, Martin Harrow and Thomas Jobe followed the long-term outcomes of patients diagnosed with schizophrenia. They reported in 2007 that at the end of fifteen years, among those patients who had stopped taking antipsychotic drugs, 40 percent were judged to be in recovery; this compared to only 5 percent in recovery among those who had remained on antipsychotic drugs. Harrow and Jobe continued to follow up these individuals, and at twenty years, they reported: “While antipsychotics reduce or eliminate flagrant psychosis for most patients with schizophrenia at acute hospitalizations, four years later and continually until the twenty-year follow-ups, patients with schizophrenia not prescribed antipsychotics had significantly better work functioning . . . . The longitudinal data raise questions about prolonged treatment of schizophrenia with antipsychotic medications.”
Harrow and Jobe’s findings were completely ignored by the mainstream media until brought to public attention by journalist Robert Whitaker in his 2010 book Anatomy of an Epidemic, and then completely dismissed by psychiatry for being merely longitudinal findings. However, the RCT “gold standard” was applied to this same issue by researcher Lex Wunderink, reported in 2013 in JAMA Psychiatry. In Wunderink’s study, patients who had been assessed to have recovered from their first psychotic episode were randomly assigned either to standard medication treatment or to a program in which they were tapered off the drugs. At the end of seven years, the recovery rate for those who had been tapered off the antipsychotic drugs was 40 percent versus 18 percent recovery for those who remained on them.
Why is Criticism of the Medical Model Taboo?
While it is not taboo to report psychiatry’s poor treatment outcomes, it is taboo to blame these poor outcomes on psychiatry. Former NIMH director Insel has repeatedly acknowledged psychiatry’s poor treatment outcomes, but he does not blame psychiatry for it in his 2022 book Healing. He states, “First, most people who would and should benefit from treatment are not receiving care.” However, more people are in treatment than ever, and as the New York Times reported in 2021, outcomes have gone in the “wrong direction.” Insel also tells us that “although individual treatments work, they are rarely combined to provide the kind of comprehensive care that most people need.” However, nobody, including Insel, argues that such “comprehensive care” has worsened, yet outcomes have worsened with more treatment.
Why is it not taboo for the mainstream media to report treatment outcome failure, the jettisoning of the serotonin imbalance theory of depression, and the invalidity of psychiatry’s DSM diagnostic manual? The public is simply being prepared for new treatments, new theories, and new diagnostic manuals—none of which fundamentally threatens the ruling class and ruling institutions of society.
However, it remains taboo to challenge whether or not medicalizing our emotional suffering and behavioral disturbances is the best model of care. Such a challenge, as noted, is not only an existential threat to establishment psychiatry but a financial threat to Big Pharma and a mainstream media dependent on Big Pharma advertising dollars. Even more significantly, such a challenge is a political threat to the ruling class which prefers “individual defect” explanations for emotional suffering and behavioral disturbances—rather than explanations that take seriously the direct and indirect effect of an alienating and dehumanizing society.
While researchers have not linked any psychiatric condition to neurobiological variables, there are many links between these conditions and socioeconomic variables. Results from a 2013 national survey, issued by the U.S. government’s Substance Abuse and Mental Health Services Administration (SAMHSA), provide extensive evidence that unemployment, poverty, and involvement in the criminal justice system are highly associated with depression and suicidality.
Moreover, in the late 1990s, the Adverse Childhood Experiences (ACE) study revealed a powerful relationship between childhood trauma (including physical and emotional abuse) with later adult emotional difficulties and behavioral disturbances. An alienating and dehumanizing society such as ours that creates extensive anxiety, powerlessness, resentment, and rage is a society that creates adults who, in their interactions with children, have little frustration tolerance; and this lack of frustration tolerance makes abuse and trauma of children more likely—resulting in the adverse childhood experiences that create later adult emotional difficulties and behavioral disturbances.
The ruling class could not care less whether psychiatric treatment consists of bloodletting, lobotomy, electroshock, SSRI antidepressants, or psychedelic microdosing. As long as the “ruling idea” of society is that our emotional difficulties and behavioral disturbances are caused by our medical defects, this keeps us diverted from just how much shit we have to eat in order to survive and how extraordinary our good luck need be for us to find joy.
As Marx stated, “The ideas of the ruling class are in every epoch the ruling ideas,” and you would have to be an especially stupid member of the ruling class not to see the value of the “ruling idea” that emotional suffering and behavioral disturbances are the result of medical individual defects—and not the result of a society that is a good deal for the ruling class but is alienating and traumatizing for many of the rest of us.