
Photograph Source: chaddavis.photography – CC BY 2.0
Privatization of public programs such as Medicare and Medicaid has been proceeding rapidly in recent years with little coverage by the media of its harms to patients, the public and taxpayers. This article has four goals: (1) to bring brief historical perspective to this trend in the U. S.; (2) to shed light on the experience over the last 12 years of profiteering by UnitedHealth Group, now the largest U. S. private health insurer; (3) to describe negative impacts on our health care system; and (4) to briefly consider lessons that can be learned from this concerted and stealthy exploitation of the public interest through the corporate greed of UnitedHealth.
Brief Historical Perspective
In the U. S., there has been a long-standing myth, now a meme, that the “free market” can resolve whatever problems we have in access, cost, and quality in delivery of health care services. Touted as the “American way,” this view assumes that a private, competitive market exists in health care. This has long been discredited for several reasons—patients often don’t really know their needs, urgency of time is often a factor, and information is not transparent. Kenneth Arrow, leading economist at Columbia University, observed in 1963 that uncertainty would be the root cause of market failure in health care as patients and their physicians grapple with unavoidable uncertainties related to diagnosis, treatment and prognosis of illness.1
“Competition” in health care markets has not controlled prices or costs but instead typically increases them. Robert Evans, health economist at the University of British Columbia, called attention in 1997 to the natural alliance between providers, insurers, suppliers and higher-income citizens in support of private financing of health care, leaving the burden of financing care for the sick and uninsured to the public sector.2 As a result, the more private financing of health care, the more difficult it becomes to finance basic health care services for sick and lower-income people through a smaller risk pool.3
The non-profit Center for Studying Health System Change conducted a nine-year study of 12 major health care markets in its Community Tracking Study involving 60 communities, 60,000 households and 12,000 physicians. It found four basic barriers to efficiency: providers’ market power, absence of efficient provider systems, employers’ inability to push for efficiency, and insufficient competition among insurers. It concluded in 2004 that there is insufficient competition among local health care systems and that providers lack enough market power to dictate terms with insurers.4
Aside from the private sector’s dismal track record over the years, however, we have seen an ongoing increase in privatization of health care, especially targeting Medicare and Medicaid. This trend has been marked by disinformation, intense lobbying, and buying off legislators in both political parties.
Profiteering in the United States
Experience since passage of the Affordable Care Act (ACA) in 2010 has proven its failure to reduce prices and cost of health care, as shown by the profiteering of Big 6 private insurers over the last 12 years, largely through privatized Medicare and Medicaid. These data points document that failure:
+ Revenue of six giant Insurers (Anthem, Centene, Cigna, AVS/Aetna, Humana and UnitedHealth) more than quadrupled from 2010 to $1.1 trillion today.
+ Combined revenues of the 3 biggest (United, CVS/Aetna and Cigna) quintupled since 2010.
+ The Big 6 profits soared from $16.9 billion in 2010 to $60.7 billion in 2021.
+ Less than one in every ten dollars of national health care spending flowed through the Big 6 insurers in 2010; today the number has risen to almost one of every four dollars.
+ While collective enrollment in the Big 6 commercial plans increased from 84.9 million people in 2010 to 91.3 million now, there was a massive increase in enrollment from 16.9 million to 63 million in privatized Medicare and Medicaid plans.
+ Almost 90 percent of enrollment growth in Big 6 health plans has come from government-funded programs, so that we taxpayers are supporting their profiteering.5
Ironically, UnitedHealth played a leading role in arguing against health care reform in the runup to the Affordable Care Act. That it turned out to be its largest cash cow over the next ten years surprised many. The explanation, of course, is that the ACA channeled the newly insured either into subsidized marketplaces or into privatized Medicaid, which became their main artery of corporate profits.
These are ways that the public and taxpayers lose as profiteering CEOs whistle to the bank (and to Wall Street):
+ Privatized Medicare Advantage HMO plans have consistently cherry-picked the market for healthier enrollees, skimped on care, and denied necessary services.6
+ Medicare Advantage disenrolls patients when they become sicker and less profitable, especially in their last year of life.7
+ Administrative overhead for Medicare Advantage is 5 to 6 times higher than that of traditional public Medicare.8
+ Overpayments to privatized Medicaid are endemic in more than 30 states, often involving unnecessary or duplicative payments to providers.9
+ Overpayments to both privatized Medicare Advantage and Medicaid are so widespread that the five largest U. S. private insurers have been kept afloat at taxpayer expense in an increasing way.10
+ Remarkably, and still below the radar of public awareness, there is a growing effort, supported by conservatives, to extend privatized Medicare Advantage to the entire U. S. population, fueled by their (now fully discredited) belief that a “competitive” private marketplace can contain costs and improve health care.11
What lessons can we learn from this abuse of the public interest by corporate greed?
1. There is no real competition in any of this privatization.
The media have not exposed the downsides of this enveloping trend as it continues with high levels of funding to legislators to maintain its momentum. As President Biden has recently said: “Capitalism without competition is exploitation.”12
2. There is no redeeming value from this privatization, as shown by UnitedHealth Group.
It just makes health care worse, while harming patients, health professionals and taxpayers. This harm to patient care and theft of taxpayer dollars has largely slid by under the radar in both countries. The roles of the media have been more facilitative, neither critical nor investigative about the downsides of privatized public programs. Not surprisingly, the Wall Street Journal is a good example of this, heralding the success of the Big 6 private health insurers as a great success without any reservations or concern over how their money was being made.
UnitedHealth Group has become the largest of the Big 6, mainly through privatized government programs. With privatized Medicare Advantage its best cash cow, the Centers of Medicare and Medicaid Services (CMS) announced a pay raise of 8.5 percent in April, 2022, one of the biggest hikes in the history of the Medicare Advantage program. Its share price immediately jumped to an all-time high of $526.97 per share, about $500 a share higher that what it was worth when Congress passed the Medicare Modernization Act in 2003.13 Figure 1 shows how “well” it has done since passage of the Affordable Care Act thirteen years ago.14
Figure 1
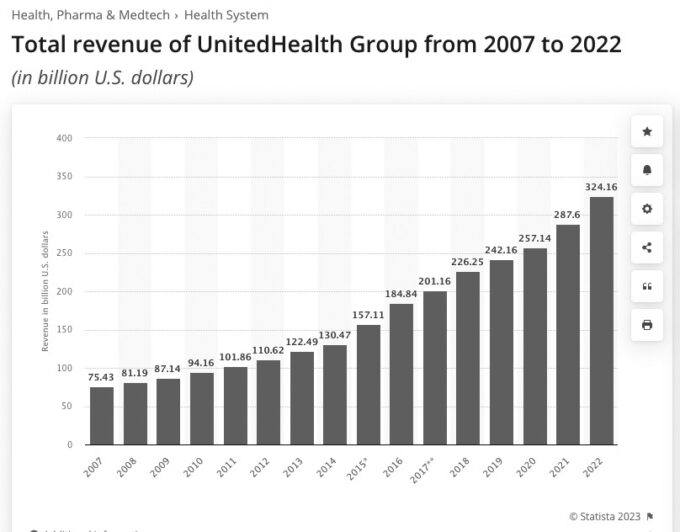
TOTAL REVENUE OF UNITEDHEALTH GROUP, 2007-2022
3. Leadership and involvement by the medical and other health professionals are important to avoiding such a widespread corporate takeover of the delivery of health care services.
Politicians, legislators, corporate executives and others outside of the health professions cannot see and care for one patient, let alone populations of people. Why should they inflict their profiteering upon those professionals who do care for people?
This is not to say that the American Medical Association has been passive in all this. It dropped out of Partnership for America’s Health Care Future, an industry front group formed to fight coverage expansions like Medicare for All, and now even allows discussion of Medicare for All. As Editor of The Journal of the American Medical Association, Dr. Howard Bauchner, wrote in 2017 in full support of health care as a human right, not a privilege. He registered his concern then that, seven years after enactment of the Affordable Care Act, there were still more than 25 million uninsured in the country and that the question of health care as a human right remained unanswered in the U. S. Moreover, he added that the success of health care reform could not be measured until that question was answered, and that a just and fair society should have health insurance for everyone.15
The American College of Physicians (ACP) has also taken a leading role toward health care reform, and has established strong collaborations with the American Academy of Family Physicians, the American College of Obstetricians and Gynecologists, the American Osteopathic Association, the American Academy of Pediatrics, and the American Psychiatric Association. As the largest delegation in the AMA’s House of Delegates, the ACP has recently published an important position paper profiling the need for fundamental reform entitled 3 Cs: Corporatization, consolidation, commodification.16
Conclusion
This 12-year story shows how the corporate greed of UnitedHealth Group propelled it to become the largest private health insurer in the U. S., largely by privatizing public programs. The results are as expected—much higher prices and costs of health care, worse access and quality of care, with increased waste and bureaucracy. The intrusion of a business “ethic” of maximizing revenue has once again trumped the traditional service ethic of health care. It exposes the essential question that continues to be unanswered in this country—who is our health care system for—patients and our population or corporate elites, Wall Street shareholders and investors? When will we answer who health care is for?
References.
1. Arrow, KJ. Uncertainty and the welfare economics of medical care. American Economic Review 53: 941-973, 1963.
2. Evans, RG. Going for the gold: The redistributive agenda behind market-based health care reform. J Health Polit. Policy Law 22: 427-465, 1997.
3. Geyman, JP. Myths as barriers to health care reform in the United States. Intl J Health Services 33 (2): 315-329, 2003.
4. Nichols, LM, Ginsburg, PB, Berenson, RA et al. Are market forces strong enough to deliver efficient health care systems? Confidence is waning. Health Affairs 23 (2): 8-21, 2004.
5. Potter, W. A decade-long look at how Big Insurance profiteers American taxpayers and the sick. Wendel Potter NOW, April 4, 2022.
6. Schulte, F. As seniors get sicker, they’re more likely to drop Medicare Advantage. Kaiser Health News, July 6, 2017.
7. Potter, W. Take it from me, tweaks won’t fix health care. USA Today, December 14, 2018.
8. Himmelstein, DU, Woolhandler, S. The post-launch problem: The Affordable Care Act’s persistently high administrative costs. Health Affairs Blog, May 27, 2015.
9. Herman, B. Medicaid’s unmanaged managed care. Modern Healthcare, April 30, 2016.
10. Schoen, C, Collins, SR. The Big Five health insurers’ membership and revenue trends: Implications for public policy. Health Affairs 36 (2), December, 2017.
11. Hilzik, M. Trump health plan a Trojan horse. Los Angeles Time, October 5, 2019.
12. Biden, The Washington Post, July 9, 2021.
13. Potter, W. Insurers’ new cash cow is the federal government’s Medicare program. The Potter Report, Tarbell, April 7, 2022.
14. McLaughlin, S. UnitedHealth Group made $287 billion last year—and is aiming even higher in 2022. Bring Me News.com, January 19, 2022.
15. Bauchner, H. Health care in the United States: A right or a privilege. JAMA 317 (1): 29, 2017.
16. Cooney, TG. 3 Cs: corporatization, consolidation, commodification. ACP Internist, March 2022.